Q: What’s been labelled the “epidemic of the 21st century” and is the fastest-growing chronic disease in the world?
A: Diabetes.
Globally, around 10% of the population live with the disease and 6.7 million people die from it each year. Despite advances in medicine, the incidence of diabetes continues to grow. The World Health Organization predicts that by 2030, diabetes will be the 7th leading cause of death worldwide.
With statistics like that, it’s very likely that if we don’t have diabetes ourselves, we know at least one person who does.
Now, we’re not experts in diabetes or medicine so this blog isn’t going to provide medical advice, talk about signs and symptoms of diabetes, how to diagnose it, or even how to manage diabetes. That’s the job of the medical professionals.
However, we are experts in habits and mindset — which affect everything in our lives including our weight, our health and the impact chronic diseases have on us.
Our aim in writing this blog is to shed some light on how habits and mindsets impact people’s lives, and how this, in turn, influences the effects of diabetes — for better or worse.
Disclaimer: General advice only. This information should not replace professional health care advice. If you’re worried about your risk of diabetes or concerned about any symptoms you may be experiencing, please speak to your health care professional.
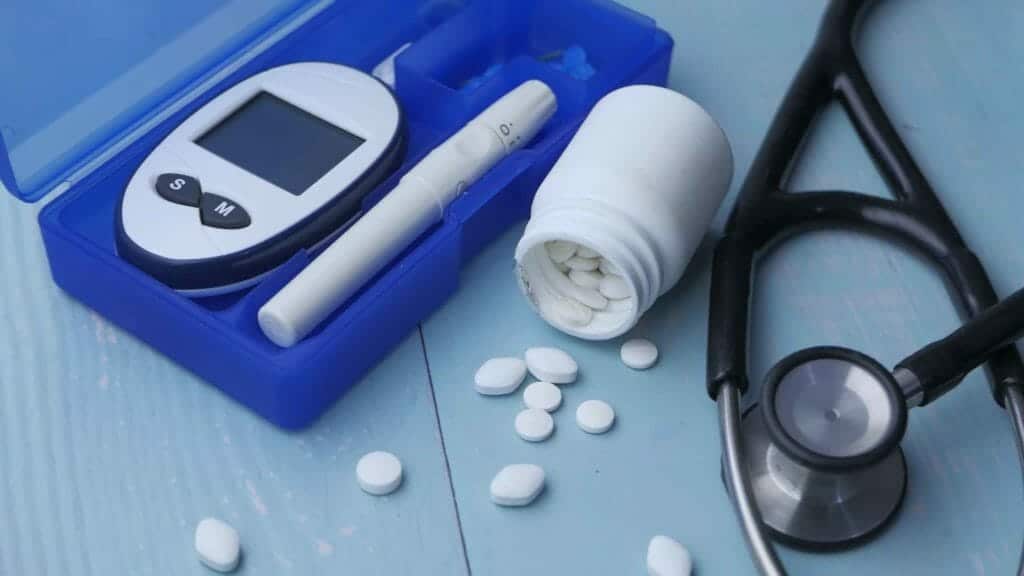
What is diabetes?
Diabetes (properly known as diabetes mellitus) is a serious condition where there is too much glucose (a type of sugar) in the blood. Unhealthy levels of blood glucose can lead to long-term and short-term health complications.
Glucose is vital for our health as it’s an important source of energy for the cells that make up our muscles and other tissues. To obtain glucose we need to convert sugars from food into energy. In normal digestion, sugar is converted into energy with the help of a hormone called insulin. Insulin is made in the pancreas (a gland behind your stomach) and is released when we eat, to help this conversion process. When insulin is released, blood sugar levels drop. As blood sugar levels drop, so does the release of insulin throughout our body.
However, in someone with diabetes, the pancreas either produces little or no insulin, or the cells don’t respond properly to the insulin that is produced. This leads to high blood glucose levels which can be harmful.
There are 3 types of diabetes:
- Type 1 — An autoimmune condition where the immune system destroys the cells in the pancreas that produce insulin. There is no cure for this and it can’t be prevented.
- Type 2 — This type of diabetes has strong genetic risk factors and modifiable lifestyle risk factors. It accounts for 85-90% of all cases of diabetes and usually develops in adults over 45, however more younger people are beginning to develop it.
- Gestational diabetes — This type of diabetes develops during pregnancy.
The type of diabetes we are referring to in this blog is type 2 diabetes.
Snapshot of diabetes in Australia
Diabetes is the biggest challenge confronting Australia’s health system. Currently, one person develops diabetes every 5 minutes. That means by the time you’ve finished reading this blog, 3 more people will have been diagnosed.
In total, about 1.8 million Australians have diabetes (any type) and as many as 500,000 have it but don’t know. For every person with diabetes, there is usually at least someone else (family member or carer) who ‘lives’ with it too. If that’s not enough, diabetes costs Australia around $14.6 billion every year.
Why is diabetes so serious?
Diabetes is a serious and complex condition, which can affect the quality of life, and life expectancy (regardless of the type you have) if it’s not well managed.
Complications arise due to the damage diabetes does to our blood vessels. Excess blood sugar reduces the elasticity of our blood vessels, causing them to narrow. This, in turn, impedes blood flow which can lead to a reduced supply of blood and oxygen. This increases the risk for high blood pressure and further damage to large and small blood vessels.
Having diabetes increases your risk of:
- cardiovascular disease such as angina, heart attack and stroke
- high blood pressure
- blindness (diabetes is the leading cause of preventable blindness in Australia)
- poor blood circulation which leads to wounds that won’t heal, infection, gangrene and even amputation
- kidney failure and bladder damage
- sexual dysfunction
- depression and anxiety
- tooth decay and gum infections
- flu or COVID-19 complications.
As you can see, diabetes isn’t a walk in the park.
What led to the epidemic?
Unhealthy diets, more sedentary work, and less physical activity have all contributed to increasing rates of overweight and obesity throughout the world. In Australia alone, 67% of adults are overweight or obese, while 25% of children carry too much weight. These high rates of obesity have been called an obesity epidemic, and diabetes is one of the major consequences.
Habits and mindset, NOT lifestyle to blame
While there is a strong genetic link with type 2 diabetes (if a blood relative has diabetes you’re at increased risk of developing it), almost 60% of cases can be prevented by maintaining a healthy weight, exercising regularly and eating healthily — things that are often referred to as lifestyle factors.
Given these lifestyle factors influence the likelihood of diabetes, it’s easy to assume that lack of exercise, eating an unhealthy diet and carrying excess weight are what causes diabetes. Unfortunately, this is not the whole truth.
The real problem is what drives people to live an unhealthy lifestyle — and this comes down to habits and mindsets.
You see people believe that they have weight problems or health problems. However, they really have personal problems (habits, mindsets, identities, beliefs and fears) that reflect in their lives.
People who develop diabetes simply have habits and mindsets that influence their lifestyle factors (nutrition, exercise and weight), which in turn increase the likelihood of them developing diabetes. These habits and mindsets also determine how much impact diabetes has on their overall health.
How habits and mindset contribute to diabetes
From a biological point of view, two of the biggest influences on blood sugar levels and whether we develop diabetes are what we eat and how physically active we are. Those who eat unhealthy diets and don’t get enough exercise are more at risk than those who eat well and exercise regularly.
One of the key reasons people fail to eat well or exercise regularly is that they don’t have time because they’re too busy. So, they skip exercise and tend to reach for quick and easy food which is often highly-processed junk food or takeaway, instead of taking the time to prepare healthy meals.
However, the reason they don’t have time is that they don’t make the time. And the reason they don’t make the time is that they struggle to put themselves first.
Instead of prioritising themselves, many people spend their time running around doing everything for other people — people-pleasing — so is it any wonder they are time-poor!
Many believe that people-pleasing is just being ‘nice’, but it actually stems from low self-worth. For example, people say ‘no’ to themselves and ‘yes’ to other people because they are afraid of upsetting them and being rejected by them. The reason they are afraid of rejection is that they fear abandonment and the reason they fear being abandoned is that their self-worth relies on other people’s approval.
We explain this in detail in our blog Our weight loss hypothesis from working with 1000s of long-term clients.
Why changing habits and mindset is essential to manage diabetes
When people are advised to manage their diabetes through lifestyle factors, many focus on eating well, getting regular exercise and achieving or maintaining a healthy weight.
While there is absolutely nothing wrong with changing exercise and eating habits, the majority of people go about it the wrong way. They turn to willpower and motivation to try to change their behaviours to reduce the effects of diabetes. While willpower works for a while, it doesn’t last forever, and then old habits take over and run their lives.
For example, someone with diabetes may decide they are going to focus on eating well, so they use willpower to do so. This might go well for a couple of weeks. However, when their boss asks them to work late, or their friends ask them to go out drinking, they’re likely to fall back into their people-pleasing habits and say ‘yes’ even if doing so means they won’t have time to prepare healthy food that week or exercise (which will ultimately lead to poor control of their diabetes). We explain this in more detail in our blog Willpower versus habits.
Where most people go wrong is they focus on changing behaviours using willpower, when they need to focus on changing the habits that lead to the behaviours. We explain this fully in our blog Habits versus behaviour: know the difference.
The truth is that unless people with diabetes change the habits that contributed to their lifestyle factors, they will always struggle to reduce the impact this disease has on them.
How changing habits and mindsets can minimise the effects of diabetes
As we have discussed, people who don’t eat well or exercise regularly don’t have time because they can’t prioritise themselves. The reason they can’t prioritise themselves is that they don’t want to upset others because their self-worth relies on other people’s approval.
Lack of self-worth is what we call a keystone habit. A keystone habit is one that leads to the development of multiple habits. In this case, low self-worth leads to people-pleasing, caring what others think, putting themselves last and a host of other habits that ultimately sabotage their weight loss and their health.
The good thing about keystone habits is that when you address them, all the other habits that are attached to them lose their power too. We explain this in our blog What’s a keystone habit and why do you have to focus on it to get results.
Let’s take an example of a person with diabetes who feels worthy.
Because they feel worthy, they don’t care what others think or need their approval.
This means they’re not afraid to upset people.
Not being afraid to upset people means they can say ‘no’ to other people.
Being able to say ‘no’ means they can prioritise themselves.
Being able to prioritise themselves means they make time for exercise, healthy eating, and doing the things they need to do to lose weight.
Making the time for healthy eating, regular exercise and weight loss means they can develop the behaviours (new habits) that ultimately minimise the effects of diabetes on their health and their life.
See how developing your self-worth snowballs into more positive actions? See how habits and mindsets can minimise the impact of diabetes?
You can learn how to build your self-worth in our blog How to build your self-worth so you can lose weight for good.
Conclusion
While you may not be able to prevent diabetes (remember, not all cases are preventable), you can take steps to minimise the effects of diabetes on your life, by changing your habits and mindsets.
Of course, for some people changing habits and mindsets so they can implement better lifestyle measures isn’t enough to keep their diabetes under control and it may be necessary for them to be on medication. Once again, every person’s situation is different and the decision to use medication should be left to the medical professionals.
However, by the same token, simply taking medication and not addressing our habits and mindsets (so we can develop better lifestyle habits) will not be enough to keep our diabetes in check, because even if we use willpower to make lifestyle changes, sooner or later, our old habits will rear their heads and run our life.
If you’re ready to make a permanent, long-lasting change to your health and your weight, we’re ready to help you.
As specialists in habit and mindset change, we can help you identify the key things that are holding you back.
If you’re ready for the body, confidence and lifestyle you desire, reach out to us and get started.